COVID-19 Mutation News You Need to Know
February 1, 2021
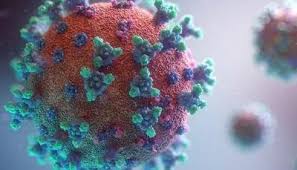
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease, undergoes random mutations (permanent genetic changes) that occur when it makes copying errors in replication (process by which it makes copies of itself to survive and spread through populations).
Like the flu and measles, SARS-CoV-2 is an RNA virus, meaning its genetic material is encoded in ribonucleic acid (RNA) instead of deoxyribonucleic acid (DNA). Unlike other RNA viruses, which have high mutation rates due to a lack of DNA polymerases (enzymes that fix copying errors), SARS-CoV-2 typically undergoes about two mutations a month, which is about one-third to one-half the rate of the flu. Most mutations do not affect the coronavirus proteins the infected cell makes.
Other mutations change a protein’s shape by altering or deleting amino acids (compounds that combine to form proteins). There are three distinct SARS-CoV-2 variants (forms of the virus) that have recently emerged due to the accumulation of multiple mutations that give the virus an evolutionary advantage.
The B.1.1.7 variant was first discovered in the United Kingdom in September 2020 and has spread to many countries around the world, including the United States and Canada. It contains 17 mutations, including the N501Y mutation, which occurs in the receptor-binding domain of the spike protein when the amino acid tyrosine (Y) replaces the amino acid asparagine (N) at position 501. The N501Y mutation allows the coronavirus to bind to the human angiotensin-converting enzyme 2 (ACE2) receptors on the surfaces of human cells more easily and infect host cells.
Another mutation is the H69-V70 mutation, which deletes the 69th and 70th amino acids in the spike protein and changes the shape of the spike protein in a way that allows the coronavirus to infect cells more successfully and makes it more difficult for antibodies to attach. Due to these mutations and a high viral load (amount of viral particles in an infected person’s blood), the B.1.1.7 variant is about 50 percent more transmissible than other variants and is projected to become the dominant variant in the United States by March.
The B.1.351 variant was first discovered in Nelson Mandela Bay, South Africa, in October 2020 and has spread outside of South Africa. The P.1 variant was first discovered in four travelers from Brazil in December 2020, who were tested during routine screening at the Haneda airport outside Tokyo, Japan. Both variants have not been detected in the United States and contain mutations in the spike protein, including K417T, E484K, and N501Y, but not H69-H70. The E484K mutation makes it difficult for antibodies produced by the immune system to recognize the coronavirus. This allows the coronavirus to reinfect people or infect vaccinated people.
Although the new variants have not been shown to increase disease severity, they increase disease infectivity, which will increase the number of coronavirus cases, hospitalizations and deaths. The Centers for Disease Control and Prevention (CDC) has launched the National SARS-CoV-2 Strain Surveillance program in November 2020, which aims to expand genomic sequencing and increase the availability of genomic surveillance data.
To mitigate the adverse effects of the variants on the pandemic, people should comply with public health protocols such as mask-wearing, vaccination, social distancing and hand hygiene. This will decrease the spread of SARS-CoV-2 and protect public health.